A history lesson!
- 1948 NHS launched – focus on provision.
- NHS & Community Care Act 1990 – purchaser provider split, GP fund-holding
- 1997-2010 reforms under New Labour… PCGs, PCTs and purchasing moves to commissioning
- Payment by results, “market” conditions, choice at patient level, competition, Practice Based Commissioning (PBC). SHAs, Hospitals and Primary Care
- Health & Social Care Act 2012 – NHSE/ area teams/evolution of clinical commissioning
- CCGs evolved from PBC. More localised commissioning. 2014 FYFV
- CSUs (Commissioning Support Units).
- CCGs encouraged to work with Local Authorities to join up Health and Care
- ICSs/ICPs emerge to as commissioners and providers and encourage CCGs to work together more strategically
- PCNs emerge to support more localised and joined up commissioning and provision
What do we hear about and see?
- NHS and Social Care is challenged
- Funding and affordability
- Outcomes are questionable and Health inequalities are not reducing
- Demand and expectations are increasing The Systems don’t link up as we would like them to
- We don’t use the data we have to the best effect
- We are unclear as to where accountability sits
So could we look at the system in a different way?
Looking at the system in a different way?
The definition for Population Health Management (PHM) recognises that health and wellbeing is more than just being ‘without disease’. It moves away from managing disease in silos to an approach based on defined populations of people, who may have multiple ‘disease conditions’.
PHM is a whole system approach, where Commissioners and Providers work together to define, measure and improve population outcomes. This represents a move away from organisational silos towards more Integrated Care, where all Providers work together to design, organise and integrate the full cycle of care around the needs of a population group, across different care settings. PHM is also supported by a strategic approach to commissioning which measures and values delivery of key outcomes for defined population segments, rather than the traditional emphasis on processes, pathways and activities.
These two elements are mutually dependent and the system of Commissioners and Providers work in tandem to prevent either element from running too far ahead or being stalled by the rest of the system.
So what is PHM?
Definition – “PHM means the proactive application of strategies and interventions to defined groups of individuals across the continuum of care in an effort to improve the health of the individuals within the group at the lowest necessary cost”
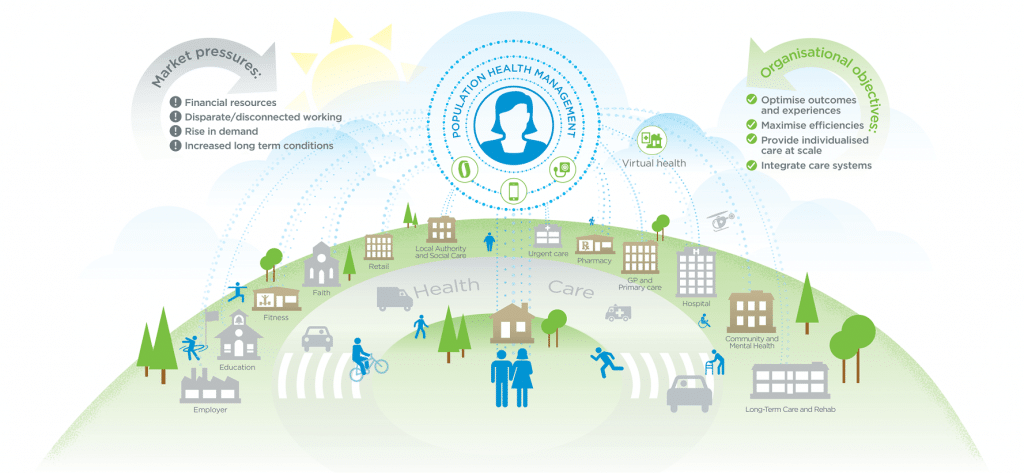
Design health and care provision around the needs of patients as opposed to disease components with greater emphasis on prevention and self care
- Connect better with patients and citizens who are proactive in the design, management and delivery of their own care
- Take proactive steps to meet the funding gap in health and social care by removing the duplication and investing in prevention
- Fully utilising informatics solutions to direct care interventions to where they are most needed, and better support professionals in joint working
So where do PCNs fit in?
In order to support the change to commissioning for outcomes, it is necessary to divide up or ‘segment’ the population into reasonable sizes that are large enough to facilitate change but small enough to test the approach
- Selecting a population segment will mean that service components could be pooled and outcomes will be developed for that segment and provide an opportunity for PCNs to plan with a group of providers in a way that they will be jointly accountable for delivery
- A key principle is that whole person needs are able to be addressed for example physical, mental health and wellbeing and social needs
- The ultimate aim is for the new system to move to commissioning for population outcomes and integrated provision for the all the segments. Selecting a segment allows the approach implemented and tested
- Segments. Frailty? Children? More than one LTC for a more joined up approach?
You might not need to start from scratch!
Work with your providers and encourage joint working
- Describe your model of care. Build on your developments. Year of Care. Primary Care Home?
- Look at your data, does that help you as to where to start? Some new ways of working might be moving this way now ? Social prescribing?
- Who else needs to be around your PCN table?